Endometriosis: A Multifactorial Disease. Wait, what?
Endometriosis as a disease is vastly complex. Although most people often refer to it as a gynecological or hormonal issue, it’s really not. Endometriosis is a systemic issue—much bigger than your pelvic cavity and so much more than a “woman’s condition”—and needs to be addressed as such.
Even more, there are some big words to describe, endometriosis! It’s heterogenous (many types) and multifactorial (many factors go into making it). It’s BIG, it’s complex, it’s so much more than a painful period.
Multifactorial is an important word, though. It means many factors go into the creation and progression of endometriosis. Nope, you didn’t just catch it like the flu—this disease took years to establish foundations and grow. Just as many factors contribute to disease, so too do many factors foster healing. This is why it’s important to know as many contributing factors as possible so that we can better manage endometriosis.
Endometriosis and Hormones
If you’ve heard estrogen is endo’s arch nemesis, it’s because, yes, endo depends on estrogen to grow. Think of estrogen as endo food that signals rapidly for lesions to grow, grow, grow, damaging healthy tissue in its wake (which, of course, invites plenty of inflammation). And, unfortunately, endo is known to be able to throw back a hefty amount of estrogen. What research has found is that endo cells are epigenetically altered to have increased levels of estrogen receptors, from a few more to a lot more (up to 140 times more!), meaning endo can gorge.
But there is also an imbalance in progesterone receptors, with endo cells observed to have low to undetectable levels. This leads to something called progesterone resistance, meaning even if there is plenty of progesterone available, your body may not be able to use it since there are little to no “docking sites.” Without the cooling power of progesterone, the effects of estrogen will be exacerbated even more. Essentially this means double trouble: lots of endo-lesion growth, barely any cooling.
The difference in receptor levels is one reason why endo may affect us all so differently, from some hormonal treatments working excellently for one sufferer and poorly for another, as well as helping explain how different types of endo behave. Indeed some sufferers with intense hormonal sensitivity may see endo rapidly spread or progress while others with low sensitivity may find their endo slow-growing. Even more, you can have different levels of receptors in different lesions within the same body (maybe yours, for example), making the hormonal discussion even fuzzier and especially reminding us why hormonal treatments aren’t able to address this disease all on their own.
Beyond hormonal receptivity, there is another element that comes into play in the localized endo environment: endo makes its own estrogen, which is obviously problematic when it feeds on it. But here comes something wild—while endo tissue may make a teeny bit more estrogen on its own, it may make up to 48 times more estrogen when provoked by inflammation! This is how inflammation may be more implicated than we realize in creating the enormous estrogen “avalanche” that endo is famous for.
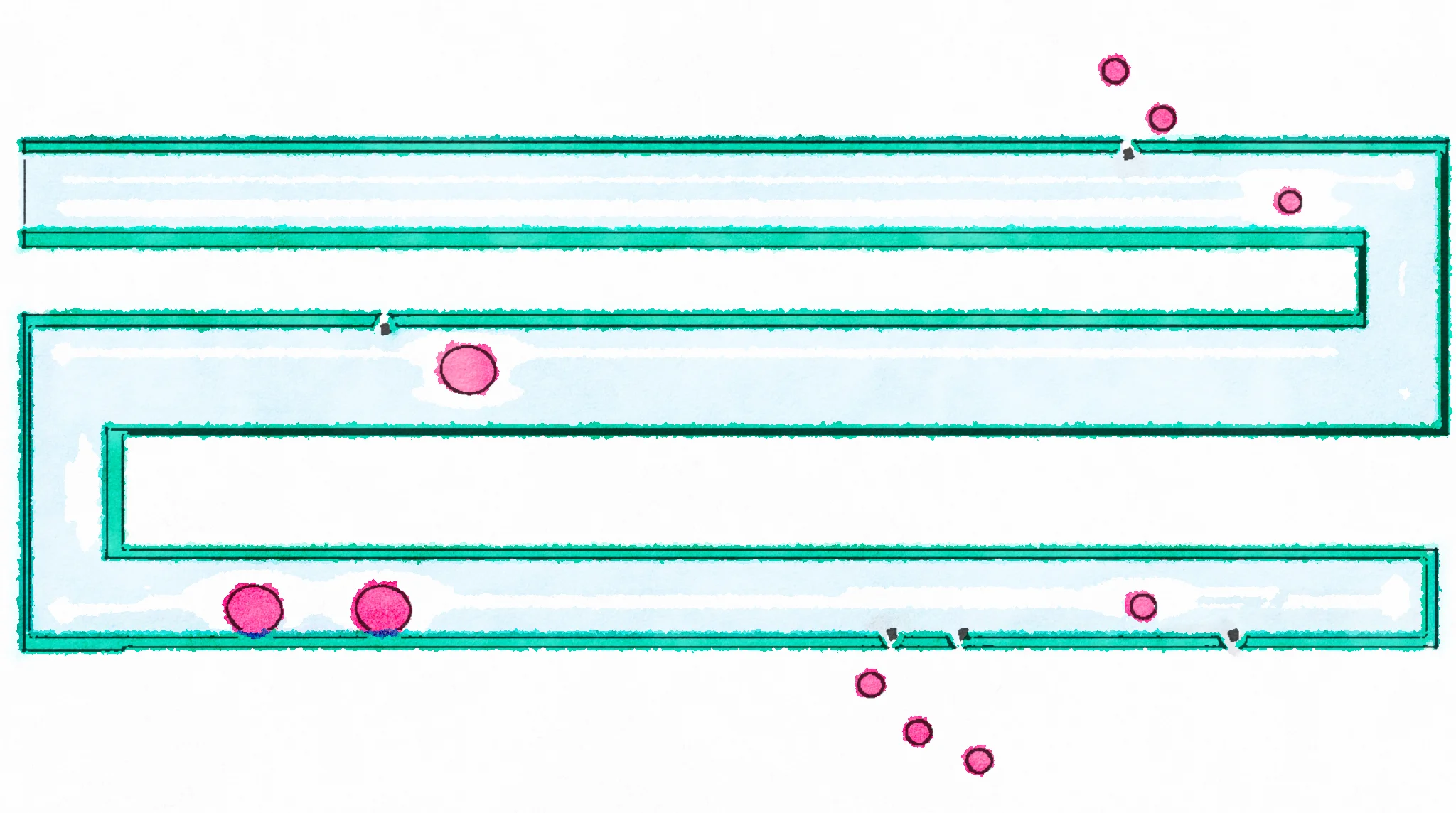
If left unchecked, this issue can become cyclical: endo eats estrogen, endo grows, growth damages tissue, damage invites inflammation, inflammation provokes endo to make more estrogen, endo eats more estrogen, and on and on. This is how the localized hormone equation becomes deeply implicated in all stages of endometriosis development, pain, and growth. It’s one of the reasons why, if left undiagnosed and untreated for too long (i.e., the 7+ years it typically takes to get a diagnosis), endo gets dramatically worse, building on itself each menstrual cycle and often resulting in worsening pain and scarring of the pelvic organs. [1-7]
The Genetic and Epigenetic Component of Endometriosis
You are born with genes inside every cell in your body, each with a specific set of instructions that inform cells how to work. This is referred to as genetics. You inherit a combination of genes from your parents, grandparents, and all your ancestors before them. Unfortunately, it’s estimated that a little over half of us (51 percent of us, to be exact) may be born with the genes that predispose us to develop endo. [8]
But endometriosis is not a genetic disease! It’s one part of the picture but doesn’t account for all endo. To understand the second part, we look to epigenetics.
Epigenetics works like this: when your genes are exposed to strong triggers, they change their behavior. These triggers can be good or bad. For example, chemical triggers can be good (exposure to lots of nutrient-rich food) or bad (household toxins), both prompting different epigenetic changes in the body. In endo, it appears there are numerous bad epigenetic alterations. These come from dioxins, phthalates, BPA, herbicides/pesticides, other chemicals, chronic inflammation, and more. Altogether, they can change the behavior of normal endometrial cells so much they end up acting like endometriosis (even when placed within the uterus!). I have a whole post on that here if you’re interested.
The Immune Component of Endometriosis
There’s a little known fact in this community that endometriosis is an autoimmune-related disease, and that the immune system of a woman with endo is improperly functioning. This is very very very important to understand.
When we think of immunity we often think of sick, or not. You might even be saying “Katie, my immune system is great, I never get sick!”. Hear me out. Your immune system is in charge of a LOT, with being sick just a fragment of how your body deals with pathogens. The other things an immune system is responsible for is inflammation, clean up, repair, attack, soothing, and more. In the endometriosis body, these behaviors appear to be misbehaving.
This is the entire focus of my book, since the immune system is so implicated in endometriosis, and I have a neat post on it here.
The Bacterial Component of Endometriosis
One thing virtually all inflammatory conditions have in common is increased gut -permeability (aka leaky gut) and/or dysbiosis. In fact, it’s widely agreed upon in science to be a pre-requisite for developing immune dysfunction. Leaky gut is when your intestinal lining has degraded so much that the insides of your intestines (aka poop-to-be) are now leaking into the insides of your body. A gross analogy? An I.V. of fecal water. You can imagine this will have an impact on your system.
And this is especially bad for the immune system, obviously, since it now mounts an immune response to bacteria, LPS, and even foods you’re eating (that are leaking directly into your bloodstream). This is a big reason for chronic inflammation and an immune system on the fritz.
Not to mention directly provoking endometriosis!
In fact, LPS alone is both a promotor and aggravator of endometriosis. Not only has it been shown to stimulate endo lesion growth, but it’s also been suggested it’s working hand in hand with estrogen to grow lesions and inflammation in the pelvic cavity. Even more, LPS was found to be 4-6x higher in the menstrual blood of women with endo, and some varieties even colonized within the endo lesions.
And as far as the endo-warrior gut, studies have shown us to have significantly altered gut microbiomes, specifically less gram positive bacteria and more gram-negative varieties (gram-negative varieties produce the LPS I mentioned). Some scientists are now hypothesizing the “gut microbiota may be involved crucially in the onset and progression of endometriosis.” This is great because it’s opening brand new doors of research that may be key in unlocking new treatment options for this multi-faceted disease, as one 2019 study posits “whether dysbiosis leads to endometriosis or endometriosis leads to dysbiosis.”
This is a very important takeaway, knowing that your “endo-belly” may be fueling the endo rather than the other way around.
I have an extensive post about that here!
The Diet and Lifestyle Component of Endometriosis
Endometriosis is not a disease of diet or lifestyle like, say, type 2 diabetes. However, like all chronic diseases, diet and lifestyle are two factors of many that go into the disease…and pretty important factors since we have a lot of control over this.
In research, endometriosis is linked to under nutrition on multiple fronts. Studies show nutrient deficiencies may even contribute to the development of endometriosis in the first place. There are also studies showing us endo-gals are either in extra need (or very deficient in) vitamin E [1,2], vitamin C [3,4], zinc [5], omega3’s [6], vitamin D [7], vitamin A[8], and selenium [9]. This may be because we’re a) not eating enough nutrients or b) because we require more nutrients than our endo-free sisters to fight the inflammation in our bodies.
I would hypothesize it’s a combination of both, since 90% of Americans are deficient in at least a handful of vitamins and minerals, and on top of that our endo-needs are higher.
Here’s a teeny-tiny example why you should care: zinc, omega-3’s, antioxidants, D, and A are all absolutely necessary for immune activities - meaning they’re needed to turn off inflammation (yes please!). If you’re severely deficient in these nutrients (which science says you probably are) then you literally won’t be able to do this, and the inflammatory response continues. It’s that simple.
In fact, the immune system is one of the biggest users of nutrients in our whole body! So if your immune system is acting out - as you know yours is - you may want to consider her like a toddler who’s hungry and throwing an angry tantrum. Please feed her :)
Stress itself is a huge player. Not only is it linked to increased gut permeability, depression, anxiety, and disease prevalence, it's also now known to increase the amount and severity of endometriosis. In a 2012 study, scientists made rats with endometriosis perform a stressful swim test 10 days in a row (omg, poor rats) to measure the bodily effects. The stress not only increased the amount of inflammation involved with the endo and surrounding tissues, it also increased the amount of endometriosis lesions!
Understanding Many Facets
To be clear, there are many more factors to endometriosis than those listed here. But I don’t want to copy and paste my whole book on this blog post.
The goal is to understand that, contrary to what you may have been told, endo did not just POP into your body. You weren’t born with endo lesions (although you can be born with an endo-like cell), and you didn’t just “get” endo from retrograde menstruation. It’s all so much more complex than that.
The exciting thing is that many of these factors are within our control. Everything from healing gut infections and reversing under-nutrition to lowering stress and removing chemicals from our lives are factors we can control today. If you need endo lesions removed, surgery would be a top priority to consider as well.
Altogether, addressing the many factors of endo means we need a holistic, full-body approach. Where to find that? On this site :) Have fun reading more on endometriosis!
1. Chen, H., Malentacchi, F., Fambrini, M., Harrath, A. H., Huang, H., & Petraglia, F. (2020). Epigenetics of estrogen and progesterone receptors in endometriosis. Reproductive Sciences (Thousand Oaks, Calif.), 27(11), 1967–1974. https://doi.org/10.1007/s43032-020-00226-2
2. Patel, B. G., Rudnicki, M., Yu, J., Shu, Y., & Taylor, R. N. (2017). Progesterone resistance in endometriosis: Origins, consequences and interventions. Acta Obstetricia et Gynecologica Scandinavica, 96(6), 623–632. https://doi.org/10.1111/aogs.13156
3. Brichant, G., Nervo, P., Albert, A., Munaut, C., Foidart, J. M., & Nisolle, M. (2018). Heterogeneity of estrogen receptor α and progesterone receptor distribution in lesions of deep infiltrating endometriosis of untreated women or during exposure to various hormonal treatments. Gynecological endocrinology : the official journal of the International Society of Gynecological Endocrinology, 34(8), 651–655. https://doi.org/10.1080/09513590.2018.1433160
4. Qi, Q., Liu, X., Zhang, Q., & Guo, S. W. (2020). Platelets induce increased estrogen production through NF-κB and TGF-β1 signaling pathways in endometriotic stromal cells. Scientific Reports, 10(1), 1281. https://doi.org/10.1038/s41598-020-57997-6
5. Noble, L. S., Takayama, K., Zeitoun, K. M., Putman, J. M., Johns, D. A., Hinshelwood, M. M., Agarwal, V. R., Zhao, Y., Carr, B. R., & Bulun, S. E. (1997). Prostaglandin E2 stimulates aromatase expression in endometriosis-derived stromal cells. The Journal of Clinical Endocrinology and Metabolism, 82(2), 600–606. https://doi.org/10.1210/jcem.82.2.3783
6. Delvoux, B., Groothuis, P., D’Hooghe, T., Kyama, C., Dunselman, G., & Romano, A. (2009). Increased production of 17beta-estradiol in endometriosis lesions is the result of impaired metabolism. The Journal of Clinical Endocrinology and Metabolism, 94(3), 876–883. https://doi.org/10.1210/jc.2008-2218
7. Bulun, S. E., Monsavais, D., Pavone, M. E., Dyson, M., Xue, Q., Attar, E., Tokunaga, H., & Su, E. J. (2012). Role of estrogen receptor-β in endometriosis. Seminars in Reproductive Medicine, 30(1), 39–45. https://doi.org/10.1055/s-0031-1299596
8. Hansen, K. A., & Eyster, K. M. (2010). Genetics and genomics of endometriosis. Clinical Obstetrics and Gynecology, 53(2), 403–412. https://doi.org/10.1097/GRF.0b013e3181db7ca1
9.