Endometriosis Pain Scale: How Bad Is It Really?
If you’re reading, clutching your phone in agony while curled around a heating pad, wondering whether your pain is “bad enough” to be taken seriously, let’s skip the suspense: it is. And it's high time you had the extra information for your doc to take you seriously. That's why this article is a straightforward tool to break down the endometriosis pain scale so you can stop wondering if you’re being dramatic (as a less-than-caring ER nurse told a client of mine, who was vomiting in pain) and start communicating your pain in ways that actually get results.
Quick Answer: What Is the Endometriosis Pain Scale?
Here’s the short version for those who have no desire to scroll through paragraphs while in pain.
The endometriosis pain scale is essentially a 0–10 rating system adapted from standard medical pain assessment tools, but tailored to the specific symptoms women with endometriosis experience. We’re talking pelvic pain, lower back agony, bowel and bladder issues, pain during sex, and that special mid-cycle stabbing sensation that makes you wonder if your ovaries purchased a knife.
Pain ratings matter because they help you:
Track patterns across your menstrual cycle—no more “I don’t know when I feel pain!”
Communicate so much better with healthcare providers—they don’t do well with general “my period hurts,” they like specifics
Push back when your pain is dismissed as “just bad periods”—show them it’s 2 weeks a month!
Build a case for further investigation or treatment, get referrals, etc.
Throughout this article, we’ll chat about what mild, moderate, and severe endometriosis pain actually feels like in real life, plus how to actually use your personal pain log to advocate for yourself in medical appointments.
One quick note, if for some awful reason you’ve heard otherwise: painful periods that make you see stars, miss work, or vomit in the ER at 3 a.m. are not dramatic—they are a medical red flag.
What Does Endometriosis Pain Feel Like at Different Levels?
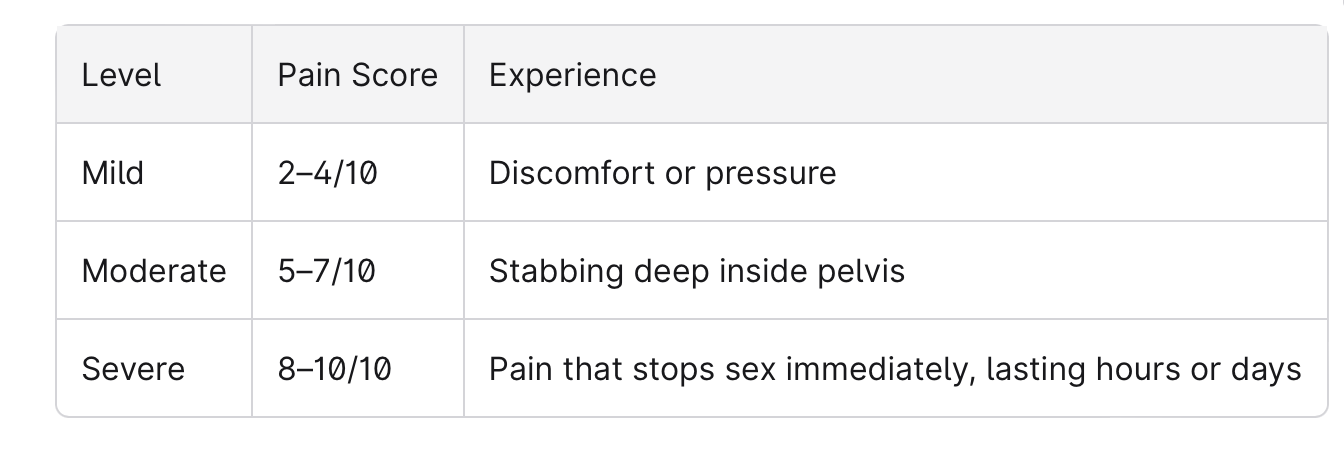
This section breaks down the rating system into real-world descriptions, because “it really hurts” doesn’t quite capture the nuance.
The truth is that pain is deeply subjective. A 4/10 for one person might feel like an 8/10 for another, depending on pain tolerance, history, and how their body processes signals. That's my reminder that this is simply a guide, not a test you can fail, and not a comparison that just because you may have less pain than another, that your pain suddenly doesn’t count as much.
Also, quick context that matters for the “is this legit?” conversation in a doctor’s office: endometriosis occurs when tissue similar to the uterine lining (often described as displaced endometrial-like cells) shows up where it doesn’t belong. That can drive inflammation, create adhesions and scar tissue, and irritate surrounding tissue—especially in the pelvis, ovaries, bowel, bladder, and around the fallopian tubes. This is part of why symptoms can be so varied, and why some people end up experiencing infertility even when imaging looks “fine.”
None of this is to scare you! All my work is about educating everything-endo. But it's just to validate that if you experience pain, your body isn’t being “dramatic.”
The main types of endometriosis pain I'll talk about include:
Menstrual cramps and period pain (obviously)
Ovulation pain (I had this the worst, personally)
Chronic pelvic and lower back pain
Pain during or after sexual intercourse
Painful bowel movements and bladder symptoms
Fatigue, nausea, and general malaise from constant pain
Later on, I will show you how to track these pain scores over time and bring them to your doctor, gynecology appointment, or endometriosis specialist. And as a general reminder, pain does not have to correlate with actual stages of endo! You can have mild endometriosis pain, for example, and stage IV (advanced) endometriosis. Or you can have
Pain Scale 0–3: Mild Endometriosis Pain
Zero is the mythical unicorn day—no pain, no twinges, and you almost forget you have a uterus! I used to cherish these, since I was more in the camp of chronic pelvic pain. But when it starts to ratchet up just a twinge, pain in the 1–3 range is mild but noticeable. Think:
Dull ache in the pelvis or abdomen
Occasional twinges around the ovaries
Low-level lower back discomfort you can mostly ignore
At this level, you can probably go to work, attend class, and focus on tasks. You might reach for a heating pad or take an ibuprofen at the end of the day, but things continue relatively normally.
Worth tracking? Absolutely. Mild pain that happens on many days of the month, or that consistently worsens around your period or ovulation, is still totally valuable data. This level gets brushed off as “normal woman stuff” far too often—even though “normal” shouldn’t mean constantly uncomfortable.
A dentist once told me something that applies here. "Your teeth should never be talking to you." Nope, you should forget your teeth are there ... and you will unless there is any pain. Same with your uterus or pelvis. There shouldn't be any conversation. If you regularly experience pain or general discomfort, but you’re still powering through, it still counts.
Pain Scale 4–6: “Moderate” Endometriosis Pain
I put “moderate” in quotations because I don’t want anyone to brush this off as normal (I just feel like moderate is such a neutral word for pain that is noticable). This is where pain starts interfering with day-to-day functioning. You can still do things, but you’re forcing it and paying for it later. It's really important to notice how much you're pushing through, as well, since this is where many of us who are trying to put on a calm face can start to erode from the inside out. Learn from me: pushing through consistently comes at a cost (oh, and also don’t take ibuprofen everyday like a multi-vitamin like I did … that’s a great way to destroy your stomach lining).
I had pelvic pain most of the time, but because doctors didn’t give me any hope (“no cure,” they said) I decided to take ibuprofen every day to keep on as usual. I didn’t want to stop living my life!! After a year of this, I had a health collapse.
Physical sensations at this level include:
Stronger cramping that demands attention
Sharp pelvic stabs that catch you off guard
Pain radiating into your lower back, hips, or thighs
Painful bowel movements or discomfort with urination
Increased bloating that is more than embarrassing, but interferes with your life
Real-life examples of how this would look: constantly changing positions at your desk, cancelling social plans because sitting upright feels exhausting, timing bathroom trips strategically, and relying on heating pads or painkillers daily.
Sex may also be painful at this level—deep penetration causing pain, either acute or that lingers. This can create anxiety or dread around intimacy, which is completely understandable.
This is really important: pain at 4–6 on most cycles, or for many days each month, is not normal and should absolutely be discussed with a healthcare provider. So many of us think we need to reach the next stage (7-10) to be taken seriously. You don't. White knuckling through your days or cycles is not normal (though it can be common, big difference), nor is it okay.
Pain Scale 7–10: Severe, Debilitating Endometriosis Pain
This is body-hijacking territory. Difficulty walking, talking, standing upright, or thinking about anything besides the pain. I personally never had a level 10 pain with endometriosis, but I did with my first labor. The pain was so intense that I would vomit every contraction, which I referred to after as something like the Cruciatus Curse (which is a Harry Potter reference; also known as the Torture Curse). A former client of mine had a level 10 pain so bad while using the bathroom that she fully fainted, landed on her face, and knocked her front tooth out.… why endometriosis is known as one of the top painful conditions. I’m trying to get across that this level of pain is not “just painful,” and we can really get across this important information by using the pain scale.
Common sensations include:
Knife-like, burning, or electric pain in the pelvis or abdomen
Pain shooting into legs, rectum, or ribs
Nausea, vomiting, cold sweats, or feeling faint
Inflammation that makes your entire body feel wrong
Real-life scenarios: doubled over on the bathroom floor, missing work or school repeatedly, ER visits for pain that mimics appendicitis or kidney stones, needing help with basic tasks like getting dressed. Sometimes this level of pain can also be very transitory: a level 9 stabbing pain that lasts 30 seconds, then back to your "normal”; a level 10 moment during sex that ebates quickly after stopping.
This level of pain, in whatever packaging it comes from for you, warrants attention. Especially if it’s new, worsening, or accompanied by fever or heavy bleeding with large clots. If you’re silently bargaining with the universe at 3 a.m. to make it stop, that’s not something to suffer through in silence. That’s something to bring to a doctor immediately.
Common Types of Endometriosis Pain (And Where They Show Up on the Scale)
As you should intimately know by now, if you follow my page, endometriosis pain isn’t just about painful periods, and not even just about the reproductive system. It can affect multiple body systems with varying intensities, which is part of why it takes an average of 7–10 years to get diagnosed. That's why, in this section, I will group pain by category and include typical ranges, so you can recognize patterns your doctor might miss.
Menstrual Cramps and Period Pain
The "most famous" symptom for many with endometriosis, period pain can begin days before bleeding starts and can last the entire period—sometimes longer. If your period pain regularly hits 5–10, or you pass large clots and soak through pads every 1–2 hours, seek medical evaluation. This isn’t normal menstruation—it’s a condition that needs investigation.
Ovulation and Mid-Cycle Pain
Endometriosis can turn mild ovulation twinges into severe, localized abdominal pain that mimics appendicitis. For me, I could feel the act of ovulation like a nuclear explosion (I knew which side was ovulating, each cycle), followed by hours of feeling the inflammation spreading through my pelvis. Pain would remain for days after, so strong I couldn't run, jump, or have intercourse. Yup, NOT NORMAL.
My pain range for ovulation was around 7; others may be less or more, from quick twinges to sudden stabbing on one side. Some people end up in urgent care thinking something ruptured. If you experience recurring intense ovulation pain, especially paired with other endometriosis symptoms, document it. “Mystery side-stabbing pain once a month” is not a fun subscription box you signed up for.
Chronic Pelvic and Lower Back Pain
This is the dull, dragging pain that hovers in the 3–6/10 range on many non-period days. It worsens with prolonged sitting or standing and sometimes feels like a permanent pre-period state.
Examples include:
Needing to lie down after work
Using cushions and lumbar support constantly
Waking at night from pelvic throbbing
Pain spreading into hips or tailbone
Even when this pain never spikes to 9/10, it affects mood, concentration, and sleep. It deserves attention—not dismissal as “just back strain.” Chronic pain plus chronic inflammation is a combo that can change how your whole body feels.
Pain During or After Sex (Dyspareunia)
Pain with intercourse should always be tracked, along with everything else
Dyspareunia is pain with penetration, deep thrusting, or aching that worsens after intercourse.
This can create fear, avoidance, and guilt around intimacy. Track when it happens-- it maybe be happening only in some positions, and on some cycle days (and knowing the pattern will help you mentally take back control, rather than thinking it's "random").
Bowel and Bladder Pain (GI and Urinary Symptoms)
Endometriosis on or near the bowel and bladder (or even just the inflammation in the peritoneal cavity) causes pain with bowel movements, urination, gas, and bloating. This may be worse around ovulation, your period, or maybe it lingers constantly (in which case I also recommend you look into SIBO).
Associated symptoms include:
Diarrhea or constipation (sometimes alternating)
Rectal pressure or stabbing pain
Feeling like you can’t empty your bladder
Bloating severe enough to change your clothing size mid-day
Pain ranges from 3–5/10 cramping to 7–9/10 stabbing with bowel movements or when passing stool or urine. Note whether GI flares align with your menstrual cycle—this can help distinguish hormonal symptoms from other conditions. These symptoms are often mislabeled as IBS alone. Gently but firmly ask providers to consider endometriosis as a contributing factor.
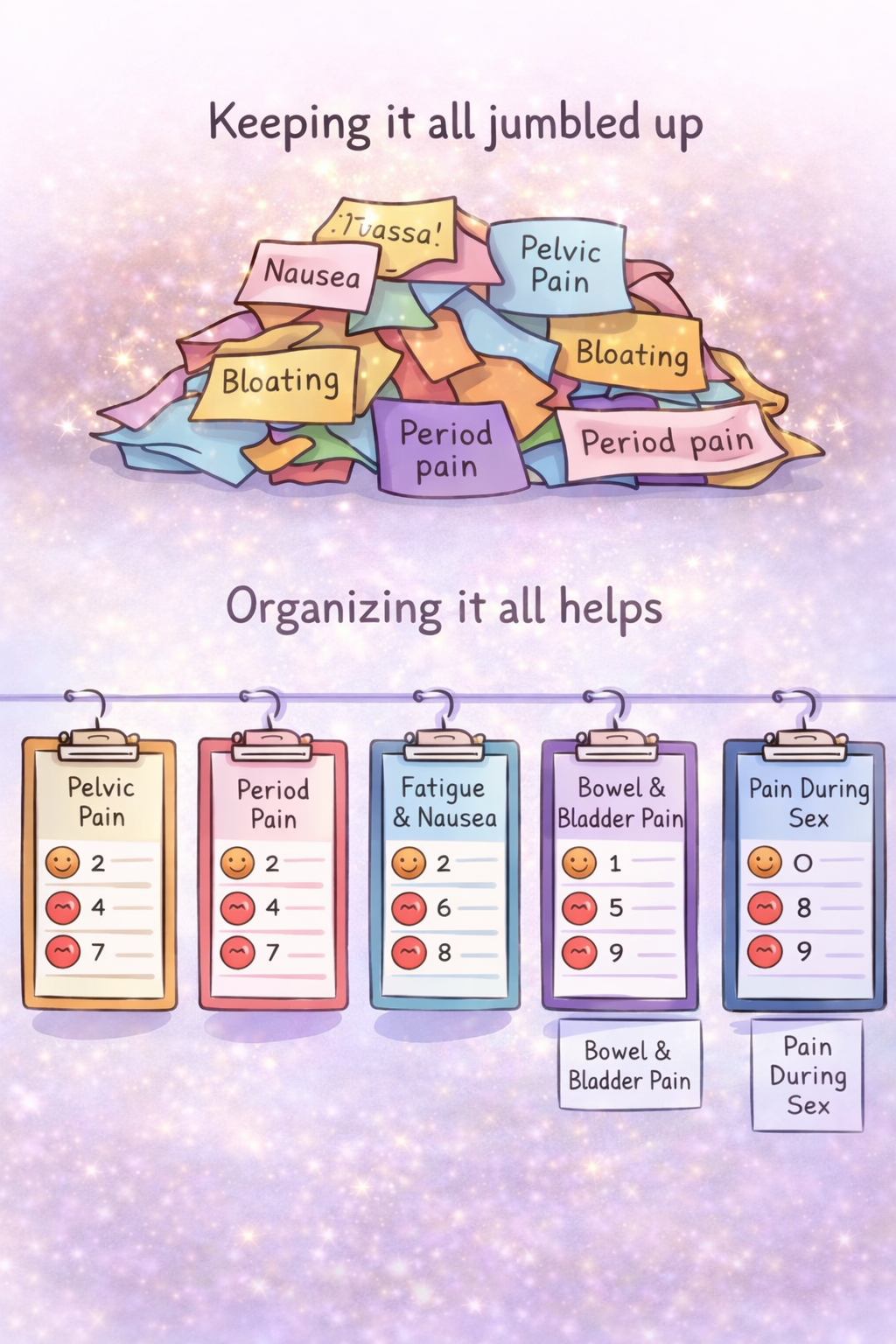
How to Use an Endometriosis Pain Scale Day to Day
Knowing the numbers only helps if you actually track them consistently. I recommend solidly tracking for at least a full cycle. Not only will this help with your doctor visits, but it also helps immensely in understanding whether healing interventions are helping as you apply them (like, is going gluten-free actually helping?). Honestly, it's so easy to forget all the twinges and stabs. I can't explain how many women I've worked with who were feeling so much better than they actually forgot how bad it "used to be" until they looked back at their tracking -- "Oh, wow, I can't believe it used to be that bad."
Suggestions for effective tracking:
Keep a daily log for at least 1-3 months
Record pain scores, location, sensation type, bleeding patterns, medication, and impact on activities
Use paper journals, phone notes apps, or period-tracking apps with custom scales
Mark “flare days” when pain rises above 6/10
Think of this as being your own private investigator.
Sample Daily Pain Log Format
If you're recording on paper, here’s a simple format you can copy:
Date: 2026-03-15
Cycle Day: Day 2 of period
Pain Score: 8/10
Location: Pelvis, lower back
Description: Stabbing, radiating
Other Symptoms: Nausea, constipation
Impact: Missed work
Interventions: Naproxen, heating pad
Another example:
Date: 2026-03-22
Cycle Day: Day 9 (mid-cycle)
Pain Score: 4/10
Location: Right ovary area
Description: Sharp twinges
Impact: Took breaks at desk
Interventions: Ibuprofen
Consistency matters more than perfection. Missing a few days doesn’t ruin the log’s usefulness.
Strategies for better appointments:
Yay! You did it! You tracked your symptoms, and now you're ready to bring your scientific observations to your doctor to get the diagnosis, referrals, imaging, or tests that you need. And with this information in hand, you have much more of a bargaining chip with your doc (and the insurance they are held by) to get you proper medical care.
Here's what you do:
Bring a printed (best, so you can hand it to the doc to look at) or digital (next best) summary of 1–3 months of pain tracking
Highlight your worst days and overall patterns (don't make them work hard to see the issues, highlight for them!)
Practice direct statements: “As you can see, my period pain is an 8/10, I vomit from the pain, and I miss work most cycles”
Leave your “I’m fine” act at home when you go to the doctor, or "I don't know, sometimes it just hurts really bad." That’s not serving you.
Practice, Practice, Practice: Phrases and Questions to Use in Appointments
Many of us are, to be honest, intimidated by doctors. Even if we don't think we are, if we get thrown a blustering, egotistical OBGYN (be they male or female, I've seen both), we may suddenly feel run over. This is why practicing helps, and I mean that literally: practice in a mirror. Literally say the words outloud. This trains you to speak up even if you feel a little nervous. Ideas of phrases that communicate urgency as well as ask for partnership:
“I need you to help me identify the cause of this pain.”
“Can we discuss endometriosis as a possible diagnosis? What are the next steps for me to concretely rule this out?"
“What referrals can you get me, because this level of pain is not manageable.”
Questions to ask:
What testing is the next appropriate step (pelvic exam, ultrasound, MRI)?
Can I get a referral to see an endometriosis specialist?
I know iron and zinc deficiency are associated with endometriosis and chronic pain. Can I get blood tests to check my levels?
Does my insurance cover pelvic floor physical therapy? Can I get a referral either way?
Another concrete suggestion of mine is to bring a trusted (and hopefully outspoken) person to your appointment for support. Sometimes it's easier to speak up on behalf of another person than to speak up for ourselves, so having a support person to help ensure you get the right questions answered can be extremely helpful.
Why Quantifying Pelvic Pain and Endometriosis Symptoms Matters (And Why It’s Not All in Your Head)
Research consistently shows endometriosis is underdiagnosed, with years passing between first symptoms and confirmed diagnosis. Using a scale and tracking symptoms provides objective-looking data in a situation that often feels very subjective and doubted. It cuts through any biased opinions of doctors or nurses who think one might be, ahem, dramatic.
The emotional side matters too. Living with chronic pain can cause anxiety, depression, and isolation. It helps us communicate to the people we love who may simply not understand when we say "it hurts."
Here’s the hopeful but realistic truth: while this condition can be life-altering, understanding your pain patterns, advocating for yourself, and building a support team can significantly change your quality of life. No toxic positivity required. Just real tools, real tracking, and refusing to stay silent about suffering that deserves to be heard. Honestly, the diagnosis is the first part of this journey.
If you’re here, though, and want to look further into endometriosis as a possibility for you, here is a quiz to generally get a better idea. Also, here is a list of less spoken of symptoms beyond pain that still very much matter.