Endometriosis Holistic Healing: A Comprehensive Guide to Finding Relief
Why Holistic Healing Matters for chronic illness, including endo
Endometriosis is not just a “bad period.” It’s a chronic, systemic disease that can hijack nearly every part of life — from energy levels to fertility, digestion to mental health. For too long, those living with endometriosis pain have been told that the only answers lie in surgery or hormonal suppression.
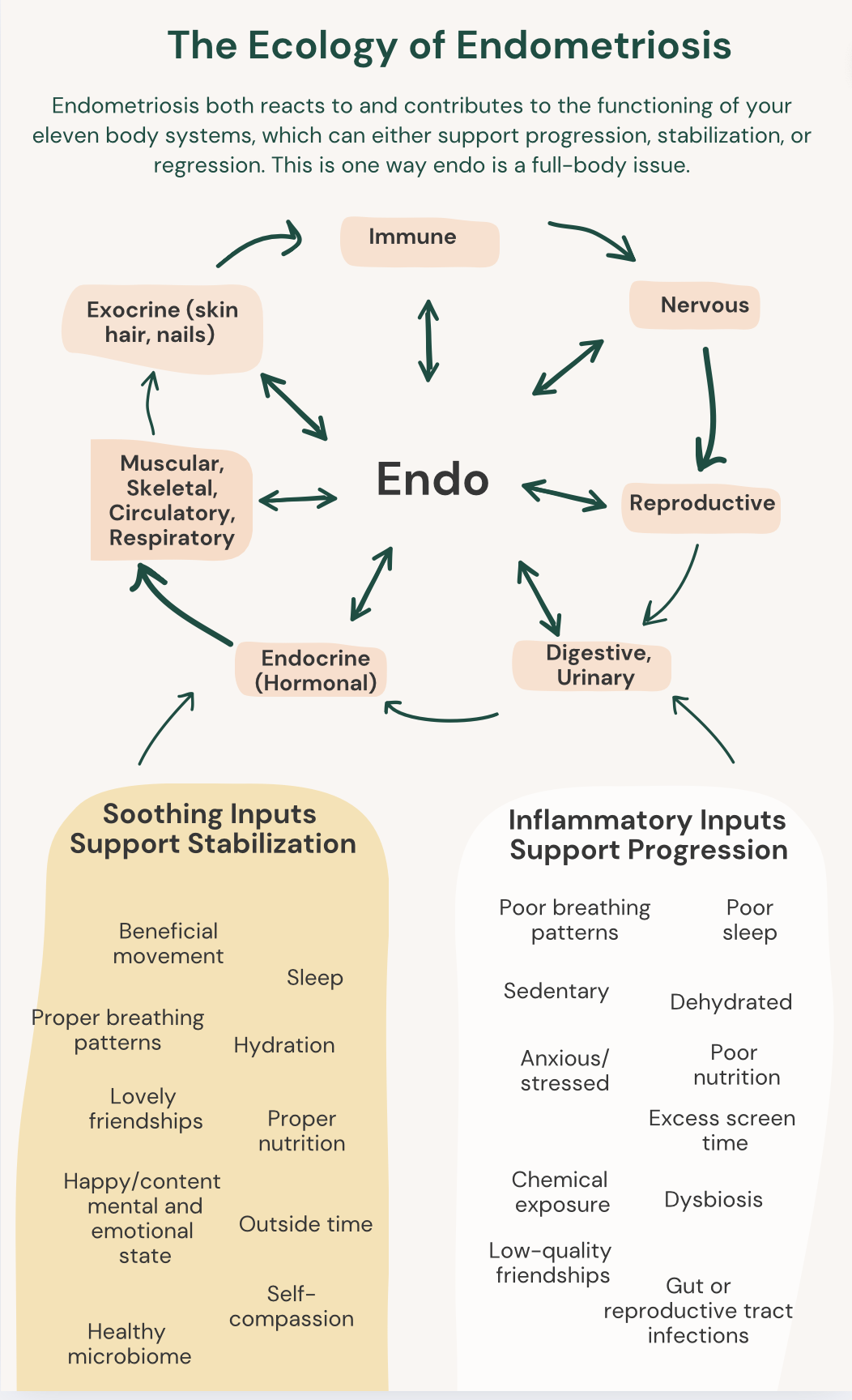
Yet growing research, along with the lived experiences of countless endometriosis patients, shows that healing requires a bigger, more integrated approach. That’s because endometriosis is not “just” lesions that “magically” appear in the body. Rather, they are a product of many factors (why endo is multifactorial), including our nervous system responses, chemical levels, nutrient sufficiency, blood sugar balance, epigenetics, inflammation levels, etc, etc. Oh, and genetics.
Understanding endo is the result of many factors (no, you are not “just” born with it, there are hundreds if not thousands of factors leading to the development of endometriosis, as I mention in my Best-selling book) we can begin to see we may need many solutions, rather than one pill or one surgery to truly feel better.
This is where holistic healing enters the conversation. By looking beyond symptom suppression and focusing on the root drivers of endometriosis lesions and symptoms alike— such as chronic inflammation, immune dysfunction, nervous system, and environmental triggers — we can begin to restore balance.
The truth is, holistic care does not mean rejecting medical treatment! Rather, it means weaving together nutrition, lifestyle, complementary therapies, and self-advocacy alongside conventional treatments to manage endometriosis in a more complete way.
This is literally what Heal Endo is all about! The goal is to help you understand your own body as a whole (the whole in holistic) and uncover what support you need to get back to health. Because that’s what you’re aiming for: being healthy, well, and whole.
In this blog, I want to help you explore the basics of how an integrative, whole-body strategy can help reduce pelvic pain, support reproductive health, and improve quality of life. Then, if you want the deeper information, I'll recommend my book to you at the end :)
What Is Endometriosis Really?
Endometriosis affects roughly 1 in 10 women — an estimated 390 million globally (although this number may be mich higher). It occurs when endometrial-like cells (similar to the lining of the uterus) grow outside of the uterus. These endometriotic cells may develop into endo lesions, which can attach to pelvic organs, the bladder, bowel, ovaries, and sometimes even distant organs such as the lungs or brain.
The hallmark experience is pelvic pain, yet endometriosis symptoms vary widely! Some may struggle with chronic pelvic pain and severe pain during menstruation, while others battle digestive distress, infertility, or chronic fatigue. In some cases, women may not experience pelvic pain at all, only to later discover advanced disease when investigating fertility challenges. I also have a blog on uncommon symptoms of endometriosis to demonstrate the variety of very random-seeming symptoms associated with endo for some. Truly, this disease is no "simple thing."
What complicates matters further is that endometriosis is not simply a gynecological issue. It is an inflammatory and immune-mediated condition. The result? Chronic inflammation, potentially scar tissue, and an escalating pain and symptoms cycle that impacts the whole body.
Moreover, endometriosis is not only progressive. In fact, research shows it’s more likely to regress or stabilize than it is to progress. How? The factor behind much of it is: inflammation. This is why our new goal is to lower inflammation in its many forms, to stack the cards in our favor when it comes to disease resilience.
Endometriosis Pain and Its Many Faces
Pain is one of the most common symptoms of endometriosis, but it does not always present in the same way. Endometriosis-related pain can show up as:
Chronic pelvic pain that persists throughout the month.
Severe pelvic pain during menstruation or ovulation.
Referred pain in the back, legs, or even shoulders.
Abdominal pain and digestive upset, often mistaken for IBS.
Painful menstruation (dysmenorrhea) with debilitating menstrual cramps.
Pain during sex, bowel movements, or urination.
Studies show that endo lesions often contain more sensory nerves than normal tissue, which may amplify pain perception. This helps explain why some with superficial disease experience excruciating pain, while others with advanced endometriosis lesions report few symptoms.
Because pain is subjective, doctors sometimes underestimate its severity. Yet when pain scores reach the highest levels, they can significantly interfere with daily activities, relationships, and mental health. Addressing this pain and symptom cycle is one of the most urgent priorities in managing endometriosis.
Endometriosis Symptoms Beyond Pain
While pain is often the first red flag, the range of endometriosis symptoms is wide and varied:
Digestive issues: bloating, altered bowel movements, constipation, or diarrhea.
Hormonal imbalances: irregular cycles, heavy menstrual bleeding, mood swings.
Fertility struggles: difficulty conceiving or recurrent miscarriage.
Fatigue: sometimes profound, bordering on chronic fatigue.
Immune dysfunction: frequent illness, allergies, or autoimmune overlap.
Mental health challenges: depression, anxiety, or suicidal thoughts.
This diversity is why endometriosis is sometimes called a “full-body disease.” It is systemic — not just about the reproductive system but deeply interconnected with immune health, nervous system regulation, and even environmental exposures.
Conventional Treatments: The First Line
For decades, conventional treatments for endometriosis have centered on three main options:
Hormone therapy or hormonal treatments – birth control pills, progestins, GnRH agonists. These aim to suppress ovulation and slow endo lesion growth. While they can sometimes reduce pain, they do not address root causes, and symptoms often return when treatment stops.
Pain medications – NSAIDs and stronger prescriptions are frequently used for pain relief. However, they often provide incomplete symptom relief and may carry side effects over time.
Surgery – wide-excision surgery with an expert is considered the gold standard of medical treatment, especially for severe pain or infertility. Removing lesions and scar tissue can reduce pelvic pain and improve fertility outcomes, but recurrence is possible if underlying drivers of inflammation are not addressed.
These conventional treatments can be lifesaving for many. But for many endometriosis patients, they are not enough on their own. This is why more women are turning toward integrative, holistic care.
The Anti Inflammatory Diet: Food as Medicine
Nutrition is one of the most powerful levers in holistic healing. An anti inflammatory diet is not about strictly eliminating "bad foods" — it’s about shifting toward foods that help reduce inflammation while minimizing those that exacerbate it. It also gives the body the proper nutrients (i.e. building blocks) it needs to heal. I have a ton more articles on this site (such as this one) or in my best-selling book, but the basic synopsis is:
Anti-Inflammatory Foods That Heal:
Omega-3-rich foods with essential fatty acids like salmon, sardines, flax, and walnuts.
Colorful fruits and vegetables packed with anti inflammatory properties.
High-quality proteins to stabilize blood sugar and reduce pelvic pain.
Fermented foods that support gut health and reduce systemic inflammation.
Nutrient Dense Foods, abundant with micronutrients like iron, zinc, magnesium, and more.
Foods That Harm:
Processed foods and refined sugar.
Industrial seed oils.
Excess alcohol.
Foods contaminated with environmental toxins such as pesticides or herbicides.
A growing number of studies, including systematic reviews, show that dietary strategies can reduce symptoms, improve pain scores, and help manage endometriosis. While diet alone may not eliminate severe pelvic pain, it can lay the foundation for pain reduction and better resilience.
Natural Treatments Beyond the Plate
Food is one foundation, but natural treatments extend well beyond diet. Holistic strategies may include:
Heat therapy – warm baths, heating pads, or infrared therapy can alleviate pain during flares.
Physical therapy – especially pelvic floor physiotherapy and manual therapy to release muscle tension, address pelvic floor dysfunction, and restore mobility.
Relaxation techniques – deep breathing exercises, progressive muscle relaxation, and mindfulness-based stress reduction.
Complementary therapies – acupuncture, herbal medicine, yoga, and massage may all play a role in symptom reliefHealEndo_Preview.
These natural treatments don’t replace medical treatment but rather complement it. Together, they can help reduce pain, manage symptoms, and improve quality of life.
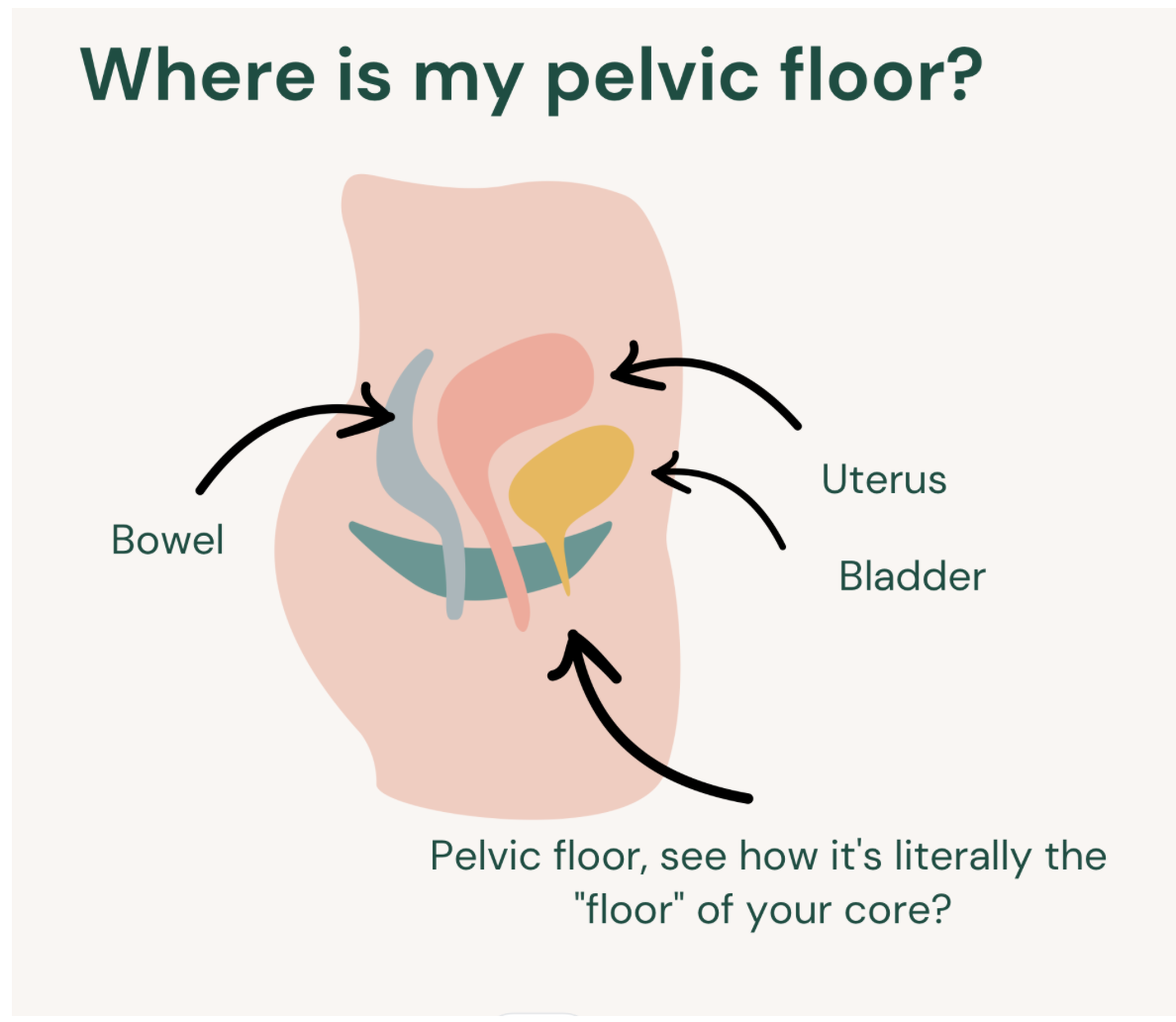
Manual Therapy and the Pelvic Floor
One often overlooked contributor to endometriosis pain is dysfunction in the pelvic floor muscles. Chronic pain can cause protective guarding, leading to muscle tension and pelvic floor dysfunction. Over time, this can exacerbate pain, interfere with sexual health, and complicate bowel movements.
Pelvic floor physiotherapy, myofascial release, and other forms of manual therapy are increasingly recognized as valuable tools in pain management. In fact, systematic reviews have shown that physical therapy can support pain reduction, improve mobility, and alleviate symptoms for many endometriosis patients.
From personal experience, pelvic floor PT helped me immensely! I had no idea the pelvic floor wasn't just the "vagina," and instead a group of muscles that can benefit from strengthening, releasing, and lengethening just like any other muscle group. If you haven't tried it, I HIGHLY recommend.
I also have more information in this pelvic floor and endometriosis blog.
Environmental Toxins and Systemic Inflammation
Modern life exposes us to thousands of chemicals daily — from plastics and pesticides to cosmetics and cleaning products. Some of these, known as endocrine-disrupting chemicals, can interfere with hormones and may even stimulate endo growth.
Research suggests that environmental toxins may worsen systemic inflammation, contributing to disease progression (I talk alllll about this in my book). Reducing toxic exposure where possible — by choosing organic foods, natural personal care products, and safer household cleaners — can help lower the burden on the immune system.
Mental Health and Chronic Illness
Living with chronic pelvic pain or severe pain month after month takes a toll on mental health. Anxiety, depression, and even suicidal thoughts are sadly common among those with endometriosis symptoms.
A holistic approach cannot ignore this reality. Addressing mental health is as vital as managing physical symptoms. Counseling, community support, and stress-reducing practices can all help alleviate the emotional load. Importantly, recognizing chronic stress as an exacerbating pain factor means that nervous system regulation must be part of any comprehensive plan.
Complementary Therapies in Managing Endometriosis
Complementary therapies are not “alternative” — they are part of a broad toolbox for managing endometriosis pain and improving quality of life. Options may include:
Acupuncture for pain reduction.
Herbal medicine for hormonal balance and reducing inflammation.
Mind-body therapies such as yoga, tai chi, and meditation.
Massage and manual therapy for muscle relaxation.
Functional Medicine to help with bacterial dysbiosis and more.
While more solid research is needed, many endometriosis patients find that complementary therapies offer meaningful pain relief and help manage symptoms where conventional treatments fall short.
Building a Holistic Plan for Managing Endometriosis
The most effective approach is often integrative — combining the best of both worlds:
Conventional treatments such as surgery and hormone therapy when necessary.
Dietary strategies like an anti inflammatory diet to address chronic inflammation.
Natural treatments such as heat therapy, physical therapy, and relaxation techniques.
Environmental detox to reduce chemical exposures, many of which are DIRECTLY associated with the creation of an endo-like cell, establishment, and progression of lesions.
Mental health support to address the emotional weight of living with chronic illness.
Complementary therapies to provide symptom relief and restore balance.
This comprehensive strategy allows each patient to tailor care to their unique needs. Managing endometriosis does not mean choosing one path — it means weaving together what works for your body to reduce pain, reduce symptoms, and reclaim your life.
Conclusion: A Hopeful Future
For too long, endometriosis patients have been told there is no cure and little hope. Yet as research and real-life stories show, holistic healing can transform what living with endometriosis looks like. From addressing chronic inflammation with an anti inflammatory diet to integrating physical therapy, manual therapy, and complementary therapies, there are countless ways to alleviate pain and restore function.
Endometriosis is not simply about suppressing symptoms — it’s about addressing the ecology of the whole body. When we reduce inflammation, support the immune system, and clear environmental toxins, we give our bodies a chance to shift. And when conventional treatments are paired with natural treatments and lifestyle changes, managing endometriosis becomes not just possible but empowering.
Holistic healing doesn’t deny the severity of endometriosis pain — it honors it. And it provides a roadmap toward real relief, resilience, and hope.
If you want to dive deeper into how to build your own endometriosis healing plan, my book Heal Endo offers a step-by-step guide backed by science and the lived experience of countless wome